Pilot report: Type 2 Diabetes Under Control with RxDiet Virtual Food Farmacy
Summary
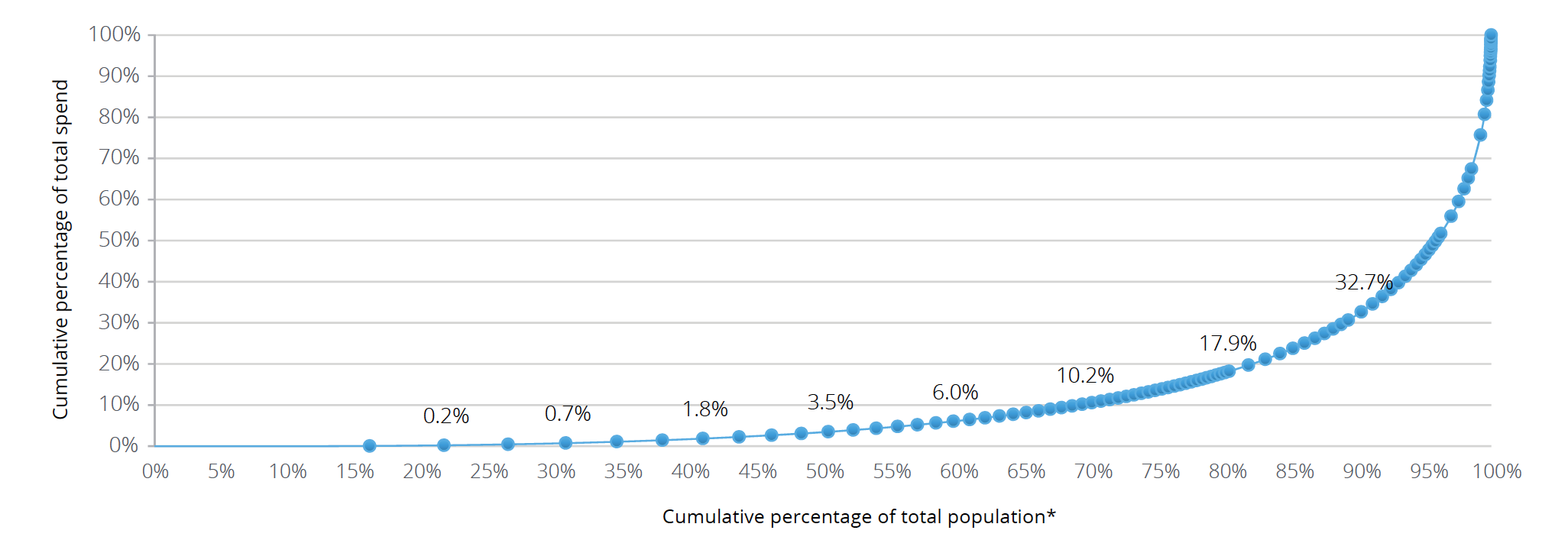
High-cost T2DM patients (top 10%) accrue approximately $52,000 more in total annual health care costs than not high-cost T2DM patients and represent a significant portion of overall healthcare spend. [1]
Novel interventions with high engagement present an alternative for patients who are not responding to traditional standard of care. RxDiet uses AI to design personalized medically tailored dietary plans and delivers ingredients directly to patients. Patients are enrolled in a 3-6month program including preparing their personalized healthy meals, health coaching and education.
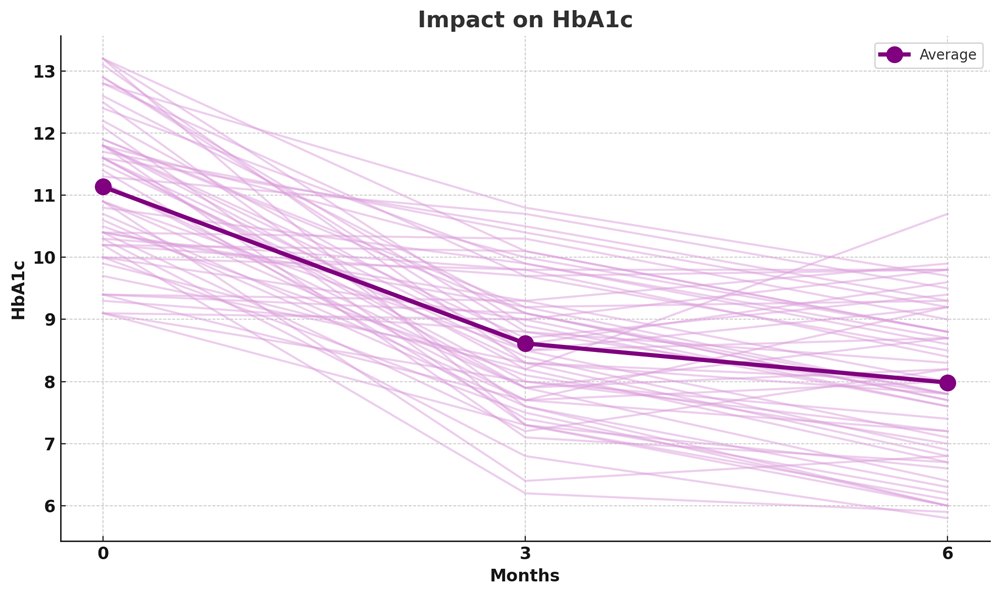
Participants with uncontrolled Diabetes Mellitus type 2 in the RxDiet Virtual Food Farmacy 6-month pilot program showed an average reduction in HbA1c by 3.16% and estimated cost savings of $48,466 per participant, significantly reducing the patients’ risk profile. This report outlines the approach used in the RxDiet pilot program, the results and economic impact.
Introduction
Chronic conditions, such as type 2 diabetes, are a significant burden on US healthcare system, with dietary and lifestyle changes often recommended as the first step in management. Despite these recommendations, most lifestyle interventions fail due to challenges in behavior modification and lifestyle adaptation. RxDiet's mission is to augment traditional chronic disease care by scaling access to dietary and lifestyle interventions using novel technology with an emphasis on complete personalization to each patient. This report provides details of the approach, and the results of the initial 6-month period, focusing on participants with uncontrolled type 2 diabetes.
Methods
Study Design
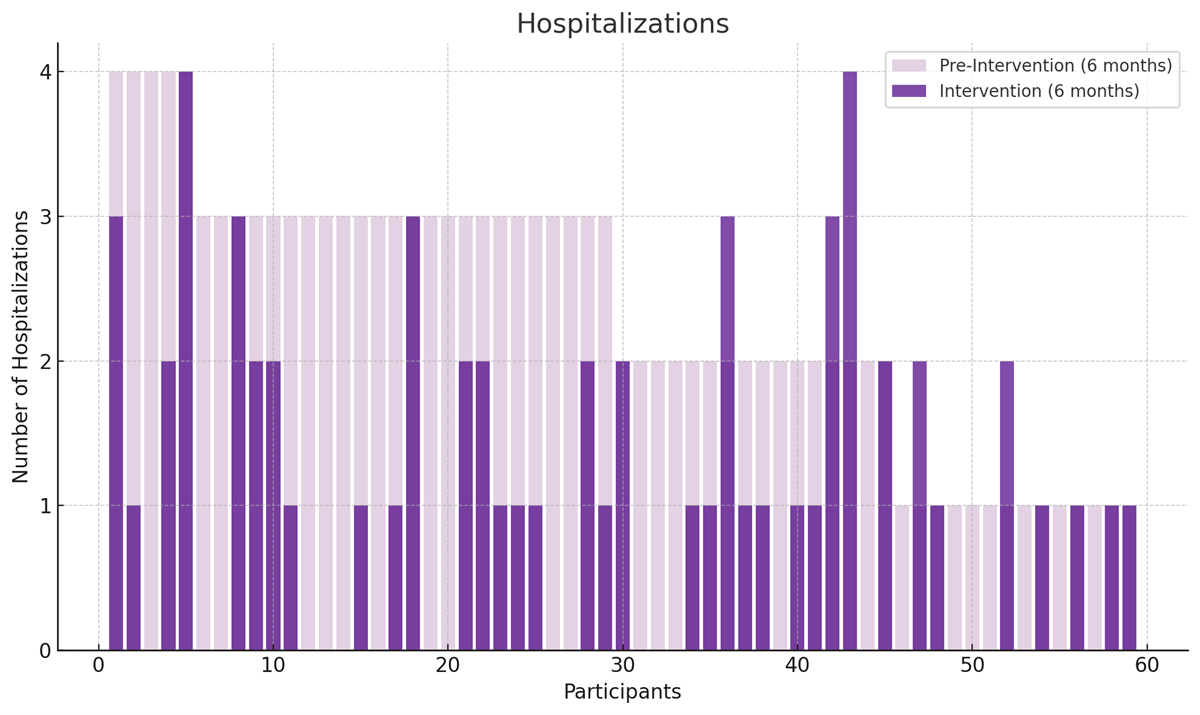
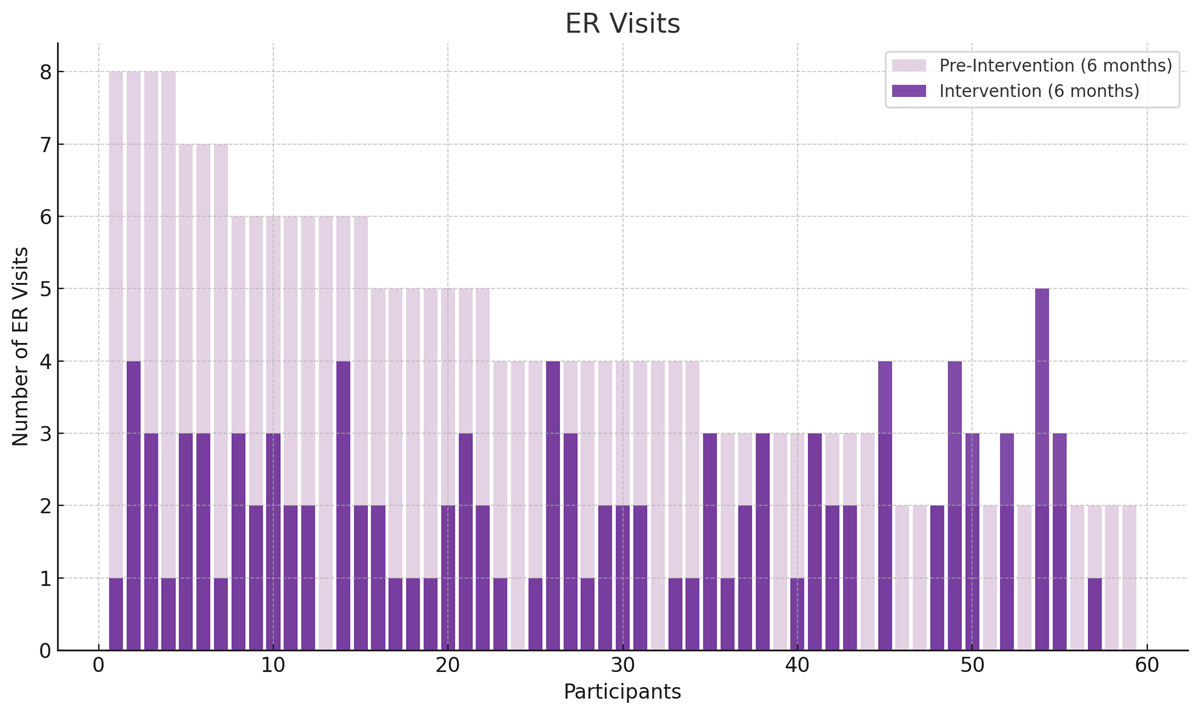
Participants were selected based on uncontrolled type 2 diabetes and healthcare utilization to be representative of the top 10% of patients regarding cost of care. Participants who completed the program (n=59) had a mean starting HbA1c of 11.1 and at least one hospitalization and two ER visits in the last 6 months. Participants engaged in a 6-month program including free-of-charge ingredient delivery and recipe instructions for 10 personalized meals per week and virtual group health coaching classes with varying frequency throughout the program. The pilot program was primarily focused on clinical impact on DMII and used HbA1c collected from 3rd party accredited laboratories and medical records as an appropriate measure.
Participants
435 potential participants were screened for uncontrolled DMII and hospitalization events in the past 6 months. 132 participants fit the criteria and 62 participants were interested to participate and able to provide access to their medical records and consents to share data with their PCP.
59 participants completed the 6-month program with 2 participants losing interest in the first 3 weeks and one participant passing away due to unrelated events.
The intervention group comprised of 59 participants, with an age range of 28 to 74 (M = 56), 54% of participants identifying as women and 46% identifying as men. Participants were located across 10 states, enrolled in Medicaid, Medicare, or dual-eligible programs. The group represented a high-acuity, medically complex population with at least 2 comorbidities to primary diagnosis of DMII and in the top 10% of DMII patients based on healthcare utilization, Charlson Comorbidity Index (CCI) ≥ 2, frequently requiring emergency care and hospitalization. [1] A criteria of at least one occurrence of hospitalization and two ER visits during the previous 6 months were used. Food insecurity was reported by 83% of participants and 68% of participants had a mental health diagnosis with 27% of participants on disability due to the underlying mental health diagnosis.
Intervention
RxDiet utilized a proprietary Machine Learning algorithm and integrations with national grocery chains to provide decentralized deliveries of personalized ingredients and recipe instructions for precisely 10 meals per week, tailored to participants’ taste preferences, ethnic preferences, portion sizes and health conditions. A unique Machine Learning model was built for each participant to best accommodate their needs, tastes, dietary prescription and available ingredients in their Zip code.
Various evidence-based dietary approaches were used based on participant preference from low-carb, ketogenic to plant-based diets, however all diets comprised of minimally processed or non-processed whole foods. The RxDiet platform adjusted preferences continuously based on participants' feedback, with a recorded cook rate of 78% for suggested recipes over 6 months with an average of 42mins spent in the RxDiet app per week by each participant. Participants were encouraged to engage in RxDiet’s structured behavioral change program, including learning sessions, support groups and health coach check-ins, as well as moderated asynchronous group communication (group chat messaging) and phone support channels. Participants were divided into groups of 12 when engaging with the learning modules and one another. Using the best practices from behavioral psychology to tailor comfortable learning and support experience to each participant. All program components were offered remotely either telephonically or over video-conferencing tools. Understanding that patient outcomes are a composite of all aspects of daily living was a key consideration. Education and discussion topics ranged from dietary habits, sleep, exercise, medication adherence, side effect reporting, and mental health to managing healthcare-provider relationships, conversations and understanding how to navigate one’s healthcare journey to achieve the best results.
Results
Clinical Results
During the period of six-month intervention, measurements of HbA1c were recorded at month 0, month 3 and month 6. Participants demonstrated a significant improvement in HbA1c levels, with a reduction of 2.48% at month 3 and 3.15% at month 6. We recorded significant reduction in hospitalizations by 1.62 visits/patient and ER visits by 1.43 visits/patient. Additionally, 87% participants reported improved medication adherence.
Economic Evaluation
RxDiet partners with health plans to administer the RxDiet Virtual Food Farmacy program for their enrollees. One of the main goals was to demonstrate economic viability and scalability of the RxDiet’s dietary intervention.
Assumptions:
- Participant group in this program is representative of the top 10% of patients with DMII in regard to healthcare cost, service utilization, and an average annual cost of care estimated at $56,000/year.[1]
- The cost of a hospitalization in this group is estimated at $28,770 with and average length of hospitalization at 9.59 days [1] and estimated cost of one hospital day at $3,000. [4]
- The cost of an ER visit in this group is estimated at $1,300.[5]
- The all-inclusive 6-month RxDiet intervention commercial cost was $1,600/member.
Savings Calculation:
Hospitalization cost * reduction in hospitalizations + ER visit cost * reduction in ER visits = total cost savings per patient
$28,770 * 1.62 + 1,300 * 1.43 = $48,466
Net cost savings:
$46,866
ROI:
30.3X
Focusing on the top 10-20% of DMII patients who form about 3-6% of total health plan population can produce favourable ROI. Additionaly, including other lifestyle-associated chronic conditions should expand the suitable intervention group to about 10-15% of health plan’s population, responsible for about 70% of total medical and pharmacy spend.[6] Focusing on reducing risk profile of this particular member group can produce significant economic impact for the health plan.
Discussion
While the small sample size limits the transferability of the findings, the rapid improvement in HbA1c and the accompanying health benefits suggest that RxDiet’s personalized dietary intervention holds significant potential for managing uncontrolled type 2 diabetes. The use of personalized AI-powered meal planning systems, and decentralized fresh ingredient delivery shows promise in overcoming barriers to dietary adherence, a first step in complete lifestyle change, healthcare engagement and patient risk profile modification.
Comparable interventions have historically showed savings between $0[2] and $192,000[3] per participant. The RxDiet intervention provides a new datapoint with a particular focus on members resistant to traditional DMII standard of care.
This pilot study focused on DMII due to a standardized and easily measurable clinical impact. However the RxDiet intervention is suitable for patients who struggle with managing lifestyle associated chronic conditions such as congestive heart failure, hypertension, cardio-metabolic conditions, chronic kidney disease and many others.
Conclusion
This case study highlights the potential for RxDiet to improve health outcomes in individuals resistant to traditional standards of care with uncontrolled type 2 diabetes and potentially other lifestly-associated chronic conditions. With further development and larger-scale trials, RxDiet has the potential to revolutionize chronic disease management and reduce healthcare costs.
References:
- Meyers JL, Parasuraman S, Bell KF, Graham JP, Candrilli SD. The high-cost, type 2 diabetes mellitus patient: an analysis of managed care administrative data. Arch Public Health. 2014 Feb 27;72(1):6. doi: 10.1186/2049-3258-72-6. PMID: 24576356; PMCID: PMC3974200.
- Doyle J, Alsan M, Skelley N, Lu Y, Cawley J. Effect of an Intensive Food-as-Medicine Program on Health and Health Care Use: A Randomized Clinical Trial. JAMA Intern Med. 2024;184(2):154–163. doi:10.1001/jamainternmed.2023.6670
- Andrea T. Feinberg, MD, Allison Hess et al. Prescribing Food as a Specialty Drug. NEJM Catalyst, 2018; 4(2). Doi:10.1056/CAT.18.0212
- Kaiser Family Foundation: Hospital Adjusted Expenses per Inpatient Day, 2022
https://www.kff.org/health-costs/state-indicator/expenses-per-inpatient-day/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D#notes
Source: (1999 - 2022 AHA Annual Survey, Copyright 2022 by Health Forum, LLC, an affiliate of the American Hospital Association. Special data request, 2023. Available at https://www.ahadata.com/aha-annual-survey-database.) - Health Cost Institute: Emergency Room Spending, Price, and Use Trends 2012-2021
https://healthcostinstitute.org/hcci-originals-dropdown/all-hcci-reports/emergency-room-spending-price-and-use-trends-2012-2021?highlight=WyJjb3N0Iiwib2YiLCJlbWVyZ2VuY3kiXQ== - Deloitte: Questioning the 80/20 rule for health care: Determining the impact for population health today
https://www2.deloitte.com/us/en/pages/life-sciences-and-health-care/articles/is-80-20-rule-of-health-care-still-true-population-value-based.html
